The Future of Global Health: Invest in Infrastructure
The COVID-19 Pandemic has shifted the ground from beneath us. Hard-earned progress in the global development sector has been set back years, and the worst inequalities that exist both within countries and at the international level have been starkly highlighted. It became clear that access to essential healthcare was not only crucial to individual survival but global health security. As noted by Doctor Michael Ryan, Executive Director of the WHO’s Health Emergencies Programme, “None of us is safe until all of us are safe.” As we move toward a post-pandemic existence, we must take on the lessons we have learned and adapt our perspective on health and where we are investing our funding.
SRI Executive’s work within the global health sector and our ongoing research into trends and challenges in this area have provided us with insight into the key areas for investment identified by experts that, if properly financed, will create lasting change. Strong infrastructure is essential, as is collaboration between the contributors in the global health architecture landscape. The quality of treatment available to patients and the speed with which vaccines could be distributed was entirely dependent on the health infrastructure in place within different countries. Though high-income countries had capacity issues within their hospitals, they had access to electricity, WASH services and safety equipment for medical professionals at a much higher-level than low- to middle-income countries. Going forward, funding must be directed specifically into strengthening this infrastructure, not only for the health and safety of those within these countries but to prevent the development of variants in diseases like COVID-19, which can have a global impact. To combat these inequalities, investment needs to be made into several areas.
Primary Healthcare
Primary Healthcare is essential to national health and requires deep knowledge of the values and cultures of local communities to ensure its effective implementation. With strong primary healthcare services in place, vaccines are more efficiently distributed, communicable diseases are more easily contained, non-communicable diseases can be identified earlier or outright prevented from developing, and the most vulnerable members of communities, such as women, children and the elderly can receive care vital to their survival. Investing in primary health care also makes financial sense, as the preventative care provided by practitioners at the primary level can minimise health spending at a national level, removing the necessity for high-cost medical interventions. Additionally, a healthy population leads directly to greater economic growth and employment levels. The African Development Bank has identified strengthening primary health for underserved populations as a key focus area for their health investment, seeking to address basic issues such as lack of water access or electricity in healthcare facilities throughout Sub-Saharan Africa. Similarly, the World Bank has emphasised the importance of primary healthcare and is pushing for a re-imagining of primary healthcare in the wake of the Pandemic, calling for countries to create tailored plans for investment in their primary healthcare systems and encouraging donors to increase their investments into this space.
Health Workforce
A necessary part of these improvements is investing in strengthening health workforces around the world. Many countries lack the number of healthcare workers necessary to provide sufficient care to their people. Investment needs to be made into increasing educational and professional opportunities, skill development, safeguarding and protection. It is not enough to simply encourage people to pursue careers within the health sector, we must also ensure they have the support systems in place to thrive in their work. A recent study found at least a quarter of the health and care workers taking part in the study reported symptoms of anxiety, depression and burnout. During the pandemic, worker burnout is estimated to have been between 41 to 52%. Healthcare professionals are the backbone of the global health sector, responsible for the on-the-ground work needed to create a lasting impact. We must invest in providing them with the tools and assistance they need to excel in their work. Furthermore, we need to provide them with monetary support that recognises the importance of their work and ensure their salaries and benefits reflect the service they provide.
Medical Manufacturing
Another key area in need of improvement is the overall manufacture and distribution of vaccines. Already acknowledged as lifesaving care, the Pandemic established vaccines as vital to our future. The speed at which vaccines for COVID-19 were developed demonstrates the outstanding work that science can deliver when provided with substantial funding. However, while vaccines were created in such a short time, their mass manufacturing, storage and distribution proved a challenge, particularly within low- to middle-income countries, leading to a major disparity in vaccination rates around the world. Though, as noted above, primary healthcare centres are part of the solution to this issue, the establishment of medical manufacturing within these countries is crucial to addressing this inequality. The African Union and Africa Centres for Disease Control and Prevention are currently calling for an increase in manufacturing capabilities throughout the continent, recognising that true vaccine equity is only possible when supply is not limited to specific regions. Of course, this will require significant financial buy-in from governments and a commitment from them and international partners to bulk purchasing of vaccines from local suppliers to ensure stability. But if successful, this investment could lead to increased employment, economic growth and significant increases in vaccination rates for numerous diseases. An overall improvement in the manufacturing and distribution of medical equipment is, in itself, a crucial step in achieving universal health coverage and eliminating existing inequalities. During the Pandemic, lack of access to equipment such as ventilators, respirators and personal protective equipment placed patients and medical professionals in unstable and dangerous situations. With strong investment into manufacturing now, the shortages and market manipulation that occurred during COVID-19 can be pre-emptively combatted in the event of a future pandemic.
manufacturing within these countries is crucial to addressing this inequality. The African Union and Africa Centres for Disease Control and Prevention are currently calling for an increase in manufacturing capabilities throughout the continent, recognising that true vaccine equity is only possible when supply is not limited to specific regions. Of course, this will require significant financial buy-in from governments and a commitment from them and international partners to bulk purchasing of vaccines from local suppliers to ensure stability. But if successful, this investment could lead to increased employment, economic growth and significant increases in vaccination rates for numerous diseases. An overall improvement in the manufacturing and distribution of medical equipment is, in itself, a crucial step in achieving universal health coverage and eliminating existing inequalities. During the Pandemic, lack of access to equipment such as ventilators, respirators and personal protective equipment placed patients and medical professionals in unstable and dangerous situations. With strong investment into manufacturing now, the shortages and market manipulation that occurred during COVID-19 can be pre-emptively combatted in the event of a future pandemic.
Pandemic Preparedness
This is the central point behind all of these recommended areas of focus, that by investing in each, not only can the overall global health system be improved, but we will be better positioned in the event of a future pandemic, which given current trends is seen as a likely occurrence. With high levels of investment and planning now, we can mitigate against the worst-case scenario for future health emergencies, particularly as the Climate Crisis continues to increase the spread of disease, malnutrition and other major health challenges, as well as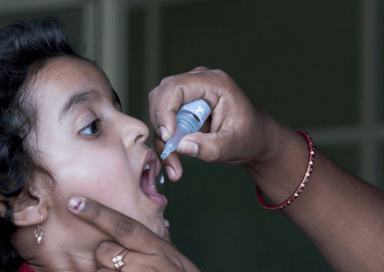 increasing the likelihood of a new pandemic emerging in the coming years. However, though there are clear areas in need of significant investment to progress health system stability globally, we must acknowledge that the economic cost of the Pandemic is likely to lead to a decrease in available funding. This, combined with the impact of the Russian invasion of Ukraine, will lead to a decline or stagnation in government spending capacity in low- to middle-income countries, per research conducted by the World Bank. In many countries, government spending is predicted to remain lower than pre-COVID-19 until at least 2027, keeping them from making the improvements to their health system necessary to combat a future pandemic.
increasing the likelihood of a new pandemic emerging in the coming years. However, though there are clear areas in need of significant investment to progress health system stability globally, we must acknowledge that the economic cost of the Pandemic is likely to lead to a decrease in available funding. This, combined with the impact of the Russian invasion of Ukraine, will lead to a decline or stagnation in government spending capacity in low- to middle-income countries, per research conducted by the World Bank. In many countries, government spending is predicted to remain lower than pre-COVID-19 until at least 2027, keeping them from making the improvements to their health system necessary to combat a future pandemic.
If we are to achieve Sustainable Development Goal Three (Ensure healthy lives and promote well-being for all ages), this needs to change. Investment and funding for health must grow, not stall or decrease. This is not an issue that can be delayed; we do not have the luxury of time. It is only by forging forward with new forms of investment, including increased private sector financing and greater funding for international improvements from high-income countries, that we can build the health system necessary for ensuring every person has access to the care they need to live long, prosperous lives and that, in the event of a health emergency, we have the foundations necessary for a powerful, global response.